Scientists at cc-TDI have uncovered a drug that turns off the key gene in childhood muscle cancer.

[Press Release] PORTLAND, OR – NOVEMBER 20, 2018 – Scientists at the Children’s Cancer Therapy Development Institute (cc-TDI) have uncovered key aspects of how the childhood muscle cancer rhabdomyosarcoma works, and in turn have repurposed a drug for breast cancer, making the drug entinostat available to children with cancer via national clinical trials.
The research went quickly, but had its start in very basic research years ago, when Dr. Keller was training with 2007 Nobel laureate Mario Capecchi in designing a genetically-engineered mouse that would get the same kind of rhabdomyosarcoma seen in children. This mouse model was described in Dr. Capecchi’s Nobel lecture. “We appreciated that the cell-of-origin for rhabdomyosarcoma influenced what treatment the tumor was sensitive to”, says Dr. Keller, senior author of the study. “Can you imagine, though, going in to your cancer doctor and she tells you, “I need to run a test for the cell of origin of your cancer. Once I have the result, we’ll know what treatments to give you. That’s exactly what our research shows in this case.”
Rhabdomyosarcoma is an aggressive tumor that originates in the soft tissues of the body – often the muscles. Rhabdomyosarcoma is the most common and deadliest soft tissue sarcoma of childhood with an unmet clinical need for decades.
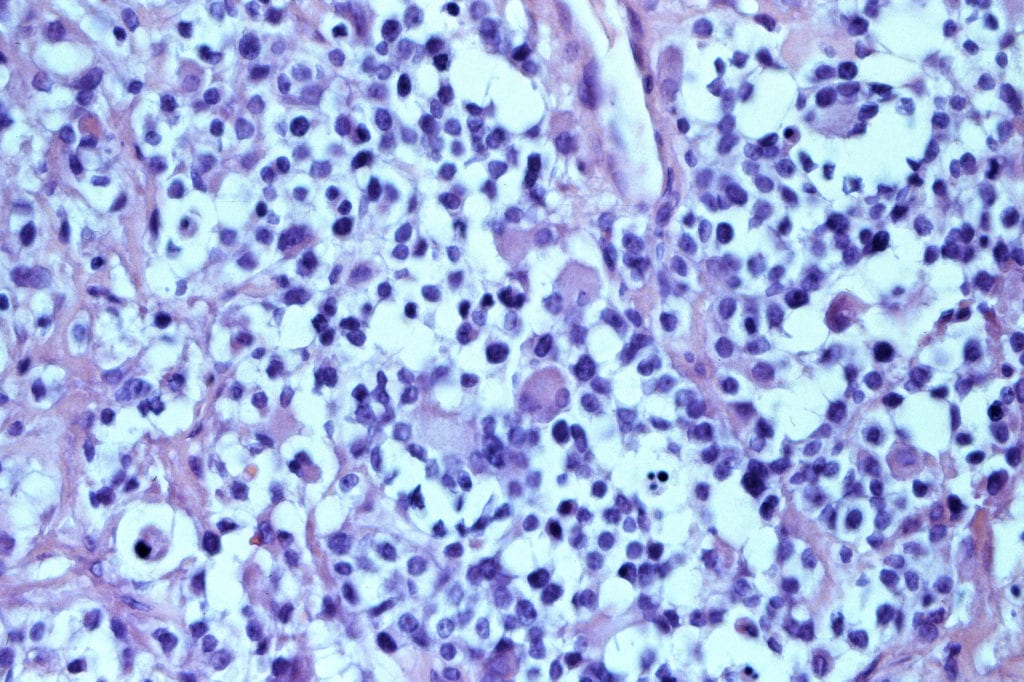
Alveolar rhabdomyosarcoma is the more aggressive subtype with survival rate less than 8% when the cancer cells associated with this disease spreads to other areas of the body. In aRMS, there is a genetic abnormality with a flip-flop (translocation) between chromosome 2 and 13 creating a fusion of two genes known as PAX3 and FOXO1, causing a fusion of these genes referred to as PAX3:FOXO1. This deadly disease does respond to chemotherapy in most cases, but the clinical challenge is preventing or overcoming recurrence after chemotherapy and/or radiation. “It’s hard to imagine that a single cancer-related fusion gene is associated with treatment resistance and a 40 to 45% decrease in overall survival,” says lead author Dr. Narendra Bharathy. “However, in 46 years, no new medicines have yet been developed that alter the often-fatal version of this childhood cancer. We are hopeful that entinostat, which turns PAX3:FOXO1 off, will provide that much needed improvement in survival for the children affected by this cancer.”
The team at cc-TDI, led by Drs. Narendra Bharathy and Charles Keller, established the effectiveness of entinostat with chemotherapy in various laboratory and mouse studies, and also found how the drug worked. Entinostat is a drug that alters the “volume switches” of genes by turning off histone deacetylases. In the case of rhabdomyosarcoma, entinostat turned off HDAC3, which resulted in less of the protein SMARCA4. Less SMARCA4 allowed increased expression of a micro-RNA called miR-27a. Increased miR-27a was important to turning off the transcript copies of PAX3:FOXO1.
“It wouldn’t be enough for our scientists to just understand how the cancer works,” says cc-TDI executive director, Molly Lindquist, a young-adult cancer survivor herself. “We needed to make sure we bridged the preclinical gap, and that the discovery could be tangible. That’s why working with the Children’s Oncology Group to get the clinical trial ADVL1513 underway was so important. You have to marvel at a basic science finding about cell of origin that results in a national clinical trial,” Lindquist says. “That families are so closely linked to our mission only accelerates our pace.”
At cc-TDI, alveolar rhabdomyosarcoma is personal as well. Biomedical engineer, Cora Ricker, joined cc-TDI because her cousin, Kiley, has a variant of rhabdomyosarcoma with a PAX7:FOXO1 gene. Cora shared, “I’ll never forget the moment I found out that my cousin had cancer. It’s one of those moments you remember exactly where you were and what you were doing. I was a freshman in college and on my way to take an exam for Introduction to Engineering class. I had no idea what I wanted to do with my life, until that moment.” Kiley’s mom, Emily Ricker Sullivan, commented” “Ever since April of 2014 when our daughter, who had just turned 5 years old, received the diagnosis of stage 4 alveolar rhabdomyosarcoma, we have been told her prognosis was grim. Our main source of much-needed hope going forward was found after speaking with Dr. Charles Keller at cc-TDI. He gave our family hope not because he said he had the answers, but because he was literally one of the few people in the world that I could find researching ways to treat aRMS. Luckily, as an added bonus, our family found that Dr. Keller also happens to be quite passionate about his work and extremely brilliant!”

“Once the shock of diagnosis wears off, one of the most gut-wrenching things to realize as a parent is that the pediatric oncology ward is full of kids suffering from the effects of their treatment rather than their disease. We strongly support research which is driving science-justified compounds into the clinic which promise fewer side effects by targeting only cancer cells. Knowing the future holds the promise of treatments like entinostat for kids with rhabdo where healthy cells are left alone while only cancer cells are hit is very exciting,” commented Sharleigh Stevenson of Braver Stronger Smarter, a supporter of the project. Dyan Ventura of dancingwithbrad.com, another supporter of the project, shared, “We lost our son, Brad, to aRMS. He was truly a shining light in our family and we miss him everyday. We are encouraged with the progress cc-TDI is making towards a new treatment for aRMS. Our family is hopeful this will spare others from enduring a devastating outcome.”
“cc-TDI is the 21st century solution to a 21st century problem,” remarks Dr. David Dilts, former Professor of Operations Management and Director of the Center for Management Research in Healthcare at Vanderbilt University. “A family-focused, team-based enterprise comprised of both biologists and engineers is what makes cc-TDI special.” cc-TDI’s unique approach and efforts towards cost efficiency and patient impact have been featured recently on NPR. The unique industrial-modern facility with links to Nike headquarters are an intriguing story as well.
Collaborators included investigators at Cold Spring Harbor Laboratory, Johns Hopkins School of Medicine, Oregon Health & Science University, Shriners Hospital for Children Portland, University of Texas Health Science Center San Antonio, Cleveland Clinic, Texas Tech University, Champions Oncology, Syndax Pharmaceuticals (manufacturer of entinostat and a sponsor of some of this research), The Jackson Laboratory, Seattle Children’s Hospital, the National Cancer Institute, the University of Pennsylvania, and Ottawa Hospital Research Institute.
This work was supported by National Institutes of Health grants 5R01CA189299; St. Baldrick’s Foundation; Braver, Stronger, Smarter Foundation; Michelle Paternoster Foundation for Sarcoma Research; dancingwithbrad.com; prayingforpeyton.com; Friends of T.J. Foundation; Clarke Gilles Foundation; and a private anonymous gift in memory of Nanette, as well as innumerable families that support cc-TDI directly through grassroots funding.
###
About Children’s Cancer Therapy Development Institute
The Children’s Cancer Therapy Development Institute (cc-TDI, www.cc-tdi.org) is a unique non-profit organization focused on the ‘preclinical gap’ in childhood cancer research. Our mission is to bridge scientific discovery and the initiation of clinical trials. Through our efforts, we will provide evidence-based testing for the selection of new drugs to be used in childhood cancer clinical trials, thus seeding pediatric Phase I and II trials. This concept was emphasized in the Institute of Medicine Report, Making Better Drugs for Children with Cancer in 2005. Our longstanding work with mouse models of brain tumors and sarcomas is the cornerstone for basic science & target discovery and our mission. The cc-TDI research team is led by Scientific Director Dr. Charles Keller who follows in the footsteps of his mentor, 2007 Nobel laureate Mario Capecchi. The cc-TDI laboratory is based on the premise of a non-profit multidisciplinary biotech and is thus located in between the Silicon Forest in Beaverton, OR (Intel Headquarters) and the Portland-area medical center. Our industrial-modern 4600 ft2 BSL wet lab facility is a former 70-year old paint factory remodeled by Nike as an off-site creative space – an ideal setting to spark innovation.